I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis with a treatment plan.
This is an online E log book to discuss our patient’s de-identified health data shared after taking his guardian’s signed informed consent.
A 27 year old male came with chief complaints of severe abdominal pain.
HOPI- patient was apparently asymptomatic 5 months back later he had a trauma where he was beaten with logs on his abdomen.
Later he developed diffuse abdominal pain which was sudden in onset, gradually progressive, radiating to back, dragging type and aggravated on food intake. Pain was associated with vomitings- almost 10 times a day which were bilious(green coloured), foul smelling, projectile and contains watery content, aggravated on taking water and relieved on medication.
After a few days he again developed pain abdomen, the pain radiating to back , then he went to government hospital where he underwent treatment but the symptoms didn't subside.
So he went to a private hospital where he took treatment but during his stay in the hospital , he tested postive for Covid. so he went to home isolation , were he approached a local rmp for the pain abdomen and covid .
After 5 days he tested negative in mid of January so he went back to the same private hospital and under went treatment and his symptoms resolved.
Later he developed pain again when he came to our hospital with the cheif complaints of pain abdomen which is intermittent , squeezing type of pain and the pain radiating to the back and also pain radiating to the left shoulder tip.
The pain is aggravated with walking, sleeping after a prolonged duration of sitting and relieves on bending forward.
Patient when complaining of pain got cect done where the impression is pancreatitis with pseudo cyst.
PAST HISTORY :-
Not a known case of dm, htn, asthma, epilepsy, tb
No previous surgical history
PERSONAL HISTORY
Diet : mixed
Appetite : decreasd since 20 days
Sleep : inadequate
Bowel & bladder : regular
Addictions :- h/0 of alcoholic intake since 5 years , regular intake of alcohol and the there is a high intake of the alcohol . he stopped the intake of alcohol 5 months back.
Family History is not significant
On Examination-
Patient is conscious, coherent, cooperative.
No pallor , Icterus,clubbing, cyanosis , koilonychia, edema.
VITALS
Temp- Afebrile
Bp-100/80 mm hg
Pr- 84bpm
Rr-16cpm
Systemic Examination -
Cvs-S1 S2 +
RS- Bilateral air present
P/A - tenderness present in epigastric region and left hypochondrium.
bowel sounds present .
CNS- NAD
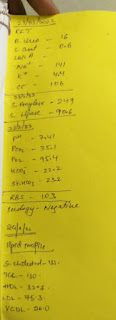
Investigations-
Treatment-
Provisional Diagnosis-
Chronic Pancreatitis with Pseudocyst.




Comments
Post a Comment