30 year old male with ALI, AKI and MI
A 30 year old male patient who is from Suryapet and a farmer by occupation presented to the OPD on 29/11/22 with
Chief Complaints of
•Vomitings and abdominal discomfort since 3 days
•SOB since 3 days
HOPI-
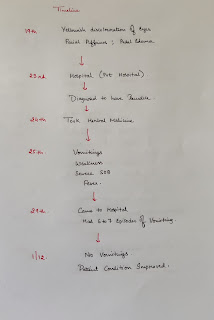
The patient was apparently asymptomatic 12 days back(19th November'22) then he developed Yellowish discoloration of eyes which was associated with facial puffiness first and followed by pedal edema which was pitting type.
Then on 23rd he went to a private hospital where he was investigated and was diagnosed to have jaundice.
On 24th he took a herbal medicine(Plants unknown) of 100 ml (half of a disposable glass) .
On 25th he developed Vomitings which were sudden in onset, 2 to 3 episodes per day initially which eventually progressed to 6 to 7 episodes per day on the day of presentation. Content was bilious vomiting (green in color) with no aggravating and relieving factors. Patient was on complete liquid diet during these 3 days.
Vomitings were associated with diffuse abdominal pain, and fever.
Fever was continuous, with evening rise of temperature and no aggravating and relieving factors.(Not associated with chills and rigor).
Patient also gave history of SOB grade 2 to 3 and Dry non productive cough.
Patient gave a history of Weight loss (>15 kgs) in the last 2 months.
Past History -
Not a K/c/o DM, HTN, TB, Asthma, Epilepsy and CAD.
Personal History -
Appetite - Decreased since 10 days
Diet- Mixed
Bowel and Bladder- Regular
Sleep- Adequate
Addictions- Used to drink alcohol once a week but since 2 months he started consuming alcohol everyday. (Whiskey- 90ml) Last binge 20 days back.
Daily routine
Drug History - Not Significant
Treatment History - Not Significant
No known allergies.
General Examination:
Patient is conscious coherent and cooperative, well oriented to time,place and person.
Thin built and moderately nourished
Pallor: Absent
Pedal edema subsided
No signs of Icterus cyanosis, clubbing , Lymphadenopathy.
Vitals
Temp:
PR: 90 bpm
Bp: 120/70 mmHg
RR: 20 cpm
Systemic Examination:
CVS:
S1 heard
Loud P2 .
RS:
Trachea central
Normal vesicular breath sounds heard
Abdomen:
No tenderness
No distension
Liver and spleen not palpable
Bowel sounds - Normal
CNS- No neurological focal deficit
Investigations-
Fever chart-
Treatment -
Inj Monocef 1gm/Iv/BDProvisional Diagnosis
• Acute liver Injury
• Acute kidney Injury
• MI
•? Sepsis













Comments
Post a Comment